Osteoarthritis, the most common form of arthritis, is a degenerating disease of the joint, characterized by cartilage destruction and associated with joint pain and swelling. For those over the age of 60, it affects 9.6% of men and 18% of women. It can occur in any joint, but most often it affects the knees, hips, hands, feet and spine.
It is generally more prevalent in Europe and the US compared to the rest of the world. Ethnicity also seems to be a factor, as African American women are more prone to knee osteoarthritis compared to caucasian women, whereas caucasians are more prone to osteoarthritis in the hip compared to those of African or Asian descent.
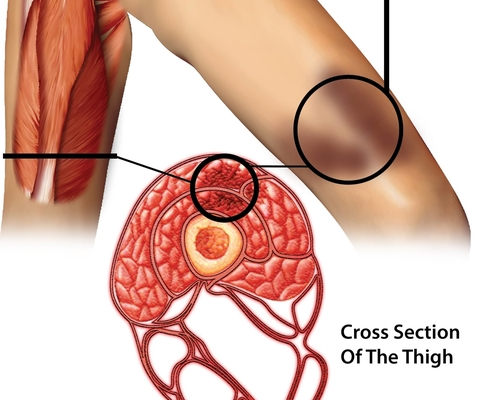
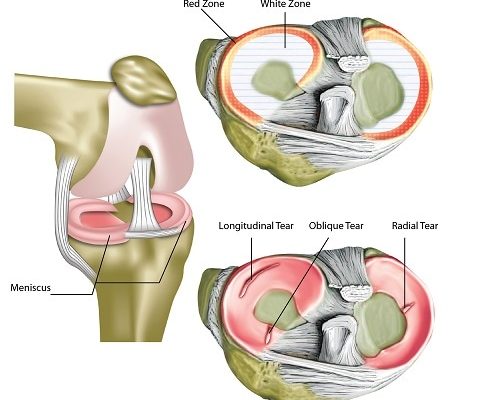
While age is the strongest factor in the development of osteoarthritis, it is a condition that can also be induced due to a traumatic injury.Post-traumaticc osteoarthritis accounts for 12% of all cases of symptomatic osteoarthritis and it mainly affects the young population. For some joints, such as the ankle, traumatic injury is the predominate factor. While all joint tissues can undergo traumatic injury, the cartilage, which plays a major role in joint protection and stabilization, is the most significant as it is irreversible and is one of the major factors for developing osteoarthritis after injury.
Football, lacrosse, rugby and hockey are examples of sports that can cause blunt trauma to the joints, and hence present high risk of joint degeneration. In a survey with responses from 185 retired football players registered in the English Professional Footballer’s Association, 47% responded that retirement was due to injury, demonstrating the high incidence rate. One-third of the respondents had already been diagnosed with osteoarthritis, while 80% reportedly experienced pain in one lower extremity joint during one or more daily activities.
In another survey with 284 respondents of former professional football players in the UK, 49% were reportedly diagnosed with osteoarthritis in at least one area, 29% reportedly had osteoarthritis in two or more sites, and 15% had osteoarthritis in three or more sites. 72% agreed with they were worried on how this would affect their future.
SYMPTOMS
Some individuals with osteoarthritis may be asymptomatic.
- Pain in the affected joint – this is the main symptom, and usually worsens when active, and gets better when at rest.
- Stiffness in the affected area – this usually occurs in the morning after getting up and gets better after 30 minutes of activity. This usually prompts an athlete or young person to seek medical attention.
- No palpable warmth.
- Joint effusion may be present. This is increased fluid in the joint.
- Bony enlargement.
- Deformity at the joint – this is usually the case of the hands and knees. For the knee, it could be presented as knock knees or bow legs.
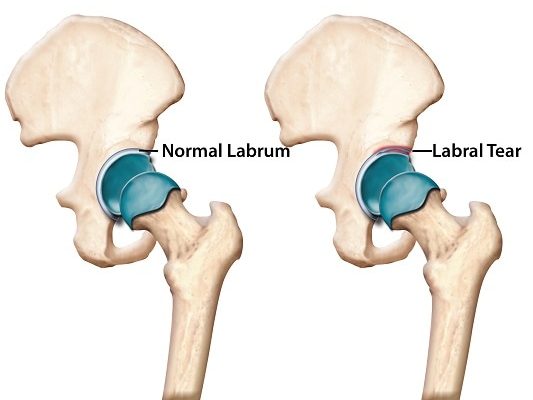
- For hip osteoarthritis, there may be formation of osteophytes or bony projections the affected joint.
CAUSES/RISK FACTORS
- Older age
- Previous knee injury
- Obesity
- Job that requires repetitive bending
- Inflammatory joint disease, such as rheumatoid arthritis
- No history of osteoporosis which is a disease where the bone becomes less dense. It has been found that those with osteoporosis are less likely to develop osteoarthritis. It is believed that this is because of reduced bone density and hence less strain on joint cartilage.
- Being female – Up to the age of 55, men and women are equally predisposed to developing osteoarthritis; however, after age 55, women are twice as likely to develop osteoarthritis compared to men. Post-menopause is seen as the reason for this increased risk.
DIAGNOSIS
Osteoarthritis is primarily a clinical diagnosis, with a physical examination of the various signs and symptoms. It is however often asymptomatic, and can only be diagnosed using an imaging technique. Experiencing pain with activity that subsides with rest is called the gelling phenomenon. Since osteoarthritis can affect any joint, physical findings may be unique to the area affected.
Pain and limitation in movement are however the most common signs. Radiography can be used as confirmation and to eliminate other possibilities. Laboratory testing is usually not necessary, and with the possibility of false positive results for tests used for gout or autoimmune (rheumatoid) arthritis, lab testing is also not recommended if physical examination and history provides sufficient evidence.
TREATMENT
Osteoarthritis is an incurable degenerative disease. Once a patient is diagnosed, most treatment therefore aim to relieve the symptoms rather than treat the disease itself. Treatment can be divided into non-pharmacologic, pharmacologic, alternative and complementary, and surgical. In general, treatment begins with the safest and least invasive methods, before proceeding to more invasive and expensive methods. Exercise should be a part of the first stage of treatment. Swimming, cycling and upper body training can help in patients who have osteoarthritis in the lower body.
For mild arthritis, acetaminophen is the preferred pharmacologic choice due to its safety and low cost. 650 to 100 mg of acetaminophen should be prescribed up to four times a day. Beyond this amount (400mg in 24 hours) may cause liver injury. If acetaminophen is ineffective, non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed. They are more effective than acetaminophen, but has a higher risk of side effects such as gastrointestinal bleeding, renal dysfunction and increase in blood pressure.
Opioids are another drug option for treatment of arthritis if NSAIDs and acetaminophen are ineffective. This, however, should be prescribed cautiously, at low dosage at first with observation for potential addiction. Steroidal injections, such as corticosteroid injections, have been found to be effective for knee osteoarthritis but not for shoulder or hand. It is usual for injections to be limited to four in one year. Hyaluronic acid injection effectiveness is still under debate, since many studies are industry-sponsored. A Cochrane review of 76 clinical trials, however, concluded that that it does improve pain and function. Another study found that corticosteroid injections were more effective short term, but less effective in the long term and this can be considered when developing individual treatment plans. Hyaluronic acid injection is, however, very costly.
Complementary and alternative medicines have also been traditionally used to help alleviate symptoms of the disease, but scientific evidence is either lacking or shows little, varying or no benefit or benefit. Acupuncture has been found to be effective only in the short term. Spa therapy has been reported to be beneficial, but a Cochrane Review that analysed these studies advised that findings be interpreted cautiously due to flaws in methodology. Capsaicin cream, derived from chili peppers, has been found to be an effective analgesic. S-adenosylmethionine, is a naturally occurring substance in the body, has been also found to be just as effective as NSAIDs in reducing disability and pain, and had a better safety profile.
Surgical treatment can be considered only if non-surgical treatment has been ineffective in alleviating symptoms. The most effective surgical intervention is total joint replacement, and has a good patient outcome. For total knee replacement, 5.4% experience post-surgery complications. Total hip and shoulder replacement also have good outcome rates.
SOURCES
[1] Woolf, A. D., and Pfleger, B. (2003) Burden of major musculoskeletal conditions, Bull World Health Organ 81, 646-656.
[2] Lotz, M. K., and Kraus, V. B. (2010) New developments in osteoarthritis. Posttraumatic osteoarthritis: pathogenesis and pharmacological treatment options, Arthritis Res Ther 12, 211.
[3] Drawer, S., and Fuller, C. W. (2001) Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players, Br J Sports Med 35, 402-408.
[4] Amoako, A. O., and Pujalte, G. G. (2014) Osteoarthritis in young, active, and athletic individuals, Clin Med Insights Arthritis Musculoskelet Disord 7, 27-32.
[5] Arden, N. K., Arden, E., and Hunter, D. (2008) Osteoarthritis, Oxford University Press.
[6] Sinusas, K. (2012) Osteoarthritis: diagnosis and treatment, Am Fam Physician 85, 49-56.
[7] Nature. Nature Reviews: Rheumatology.