What is degenerative disc disease?
Degenerative disc disease (also known as DDD or degenerative disc disorder) is a very common cause of neck and lower back pain, it is often related very closely to spondylosis.
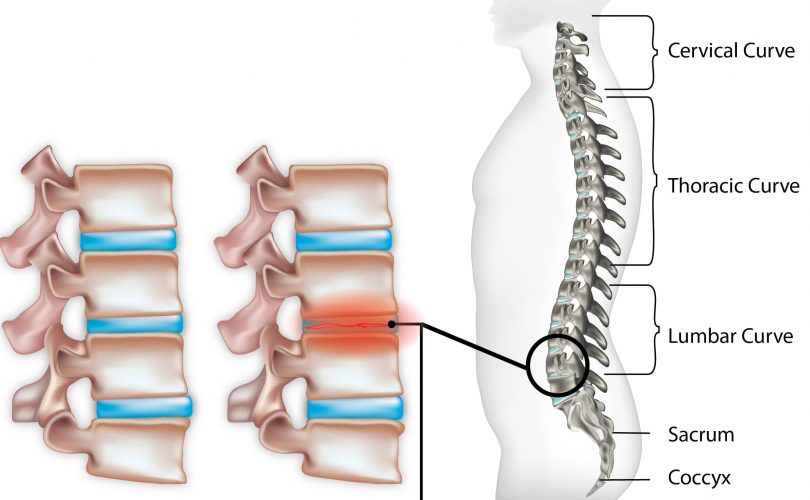
It is often characterised by the degeneration of one or more of the intervertebral discs in the spinal column. These spinal discs are soft, cartilage type tissues that act as shock absorbers in the spine whilst separating each bone that makes up the vertebrae.
These discs aid in the movement of the back, including twisting, turning and bending. Although this condition can occur anywhere in the back, the most commonly affected areas include the neck (cervical region) and the lower back (lumbar region).
DDD (degenerative disc disease) is usually a long-term pathologic process that can cause acute or long-term back pain in an individual especially if it is not treated in time. Although disc degeneration is not common in young adults as it is a disorder that occurs due to the aging process, it can affect the day to day activities of an individual and reduce their overall range of movement. The pain experienced may also prevent certain normal actions from being performed e.g. running, swimming, bending to pick up an item.

The degeneration of these discs can lead to various issues affecting the back and neck leading to added pressure on the spine and possible future nerve damage. These related issues include:
- Stenosis of the spine – narrowing of the spinal canal which aids in holding the spinal cord
- Osteoarthritis – degradation of bone cartilage that cushion and safeguard the joints and bones
- Herniated disc – protruding or breaking open of a spinal disc
Degenerative disc disease is usually characterised by radiating pain or numbness stemming from somewhere in the spinal column, usually due to a degenerated disc somewhere in the lumbar region or spinal column. Common questions that often accompany this condition include:
- Will the pain get worse as I age?
- Will the condition become crippling and will I end up in a wheelchair?
- Would the need for surgery be inevitable?
- Will I have to quit sports and activities indefinitely?
- Will other spinal discs be affected by the disease?
- Is it hereditary?
What are the causes of degenerative disc disease?
DDD (Degenerative disc disease) is a common condition that affects many people, with its main cause being related to the aging process. Due to the general wear and tear of constant use, as we age, the spinal discs naturally start to erode leading to degenerative disc diseases in the long term.
There are also other risk factors that can increase the likelihood of DDD which include:
- Cracks and tears – tine fissures in the annulus (outer layer of the spinal disc) may allow the protrusion of the soft jelly like substance found in the nucleus (disc membrane)
- Sharp acute injury – a sudden force or fall to the area which causes herniation may start up or quicken the process of degradation
- Fluid loss – if the discs are not well lubricated, then they may lose their flexibility and ability to effectively cushion the surrounding vertebrae
- Lifestyle – the chance of degenerative disc disease is increased in those with certain lifestyles, such as those who smoke, are overweight or are in a job that required heavy lifting.
- Osteophytes – when the spacing between the vertebrae bones become smaller the body reacts to this by creating bony spurs to compensate, known as osteophytes, these adversely though can put more pressure on the spinal column and lead to nerve damage
- Genetics – those with a family history of disc degeneration disease may be at a higher risk of having the condition also
- Spine biomechanics – other conditions that can affect the spine negatively such as scoliosis or osteoarthritis
What are the symptoms of degenerative disc disease
Many people can have degenerative disc disease without knowing and although the degrading disc may not cause any immediate problems, for some the pain becomes very unbearable and affects their day to day life.
It is said that the pain is due mainly because of inflammation and instability of the affected discs, due to the altered biomechanics of the back as a result of the degenerated discs there is a possibility of increased muscle spasms.
The most commonly reported symptoms of degenerative disc disease include:
- Radiating pain in the lower back (lumbar region) or neck (cervical region) after prolonged sitting.
- Discomfort or pain when participating in activities mainly involving the back muscles, e.g. lifting, pulling or twisting
- Numbness traveling down the buttocks and legs if the spinal nerves are irritated (similar to that of sciatica)
- Limited range of back movement, especially if more than one disc is heavily affected due to lack of flexibility
As the vertebrae and nerves in the spinal column are very closely intertwined, any change in the spacing of the discs and vertebrae can increase the risk of nerve irritation, which in turn can cause other spine related conditions. As the symptoms or pain experienced from this condition differs from person to person it is advised to confirm a medical diagnosis to understand the underlying cause of DDD, as pain may not be an accurate indicator or the level of disc degradation.
How is degenerative disc disease diagnosed?
The diagnosis of degenerative disc disease is usually carried out by a qualified doctor or chiropractor through a physical examination and questions to determine the spinal health of the individual.
The doctor is likely to check the range of lower back movement, flexibility and any indicators that may suggest that the spinal nerves are being affected. A look at your medical history may also be conducted with some questions asked, including when the pain first started, when it is most uncomfortable, what relieves the pain etc.
To confirm a more accurate diagnosis, the physician may also perform an X-ray or MRI (magnetic resonance imaging) scan taken to understand the extent of damage to the discs although this on its own cannot confirm degenerative disc disease
What are the treatments for degenerative disc disease?
Most medical specialists agree that improving back strength and flexibility is usually the best way to reduce back pain. Blood flow from regular exercise helps to oxygenate the surround muscles and tissues whilst removing any waste products from inflammation.
Although there is no way to stop the degradation of your vertebral discs as you age, effective conservative treatment can help to either slow the process or reduce any pain experienced, improving the overall management of the condition in the long term.
It is important to understand that having degenerative disc diseases should not have a negative impact on your well being or life, in fact many people with the condition may not experience any pain. Other treatments that compliment physical activity and therapy include:
- Medication – such as pain killers and anti-inflammatory drugs (NSAIDs)
- Heat and cold therapy – these can help in reducing or increasing blood flow around the affected region, which will assist in either reducing any inflammation or allowing for better healing of the area
- Surgery – this is usually the last resort, and only occurs when all other conservative treatment options have proved to be ineffective or the pain is unbearable. The process usually involves the replacement of the degraded disc with an artificial one. Another surgical procedure would involve spinal fusion.
- Mobilization – this involves specially formulated procedures to improve the range of movement of the back and increase overall back strength.
Recovery and prevention techniques for degenerative disc disease
In the process of recovering from a condition such as degenerative disc disease there are four steps that can be taken to ensure that the risk of reinjuring the area or worsening the condition is reduced. These methods can and are normally utilised for other soft tissue or muscle related injuries also. They include:
STAGE 1 – Protection and Pain relief
The injury is normally first identified by its symptoms, such as the pain radiating from the affected area, which is usually the main cause for seeking treatment for degenerative disc disease.
By reducing inflammation and other related causes, this can help in reducing the pain experienced. The physiotherapist is most likely going to recommend a range of treatment types from ice packs and massages to acupuncture and even adhesive tapes. All these alongside the use of NSAIDs are usually the first step towards successful recovery.
STAGE 2 –Restoring Range of Motion and Strength
As the inflammation and pain starts to subside, your physiotherapist is likely to move towards exercises and movements to restore your normal back function through range of motion and muscle strengthening techniques. A treatment plan to work on core stability may be recommended especially as it helps in [providing more stability to the spine and mid-lower back.
Intermittent stretching and massaging of the affected area may not help directly with the degenerating discs but can help in strengthening the surround muscles, putting less strain on the vertebral discs.
STAGE 3 – Full Recovery
As the dynamics of the back begin to improve and don’t occur anymore, you are likely to have any alignment of ROM (range of motion) exercises intensified. These will also continue to build on the surrounding gluteal muscles and outer core.
Depending on the exercise or sport you are involved in; your physiotherapist is likely to assess your current state and decide as to whether you are in a fit and ready state both physically and mentally to return back to said activity. This final stage of rehabilitation should be considered as important as the earlier stages to prevent any risk of regressing.
STAGE 4 – Preventing a Relapse
Although it is not possible to stop a vertebral disc from degenerating, it is possible to slow down its progress and limit the occurrence or severity of back pain. Failure to comply adequately to rehabilitative procedures is usually the main cause of reoccurrence.
During this stage, it is essential that you have regular check-ups with your physiotherapist to ensure that the biomechanics of the spin and pelvis are in good order. The importance of exercising regularly can also not be taken for granted in preventing a reoccurrence. Simple activities such as swimming, light jogging or palates can go a long way in keeping the back in good shape.