The knee is the largest joint in the human body consisting of ligaments and joints which connect the tibia (lower leg) and femur (thigh) bones. Being the critical part of the body that controls the majority of movement for any sport, the knee is most susceptible to various types of injuries.
The knee consists of two joints; one between the femur and tibia (tibiofemoral joint) and another between the femur and patella (patellofemoral joint). The surface of the bones involved are called the articular cartilage – that functions to absorb impact and provides a smooth gliding surface for joint movement, meniscus – two discs that separate the femur and tibia, ligaments, tendons and muscles that aid in the movement of the knee.
The knee is a “hinge” type joint that allows the leg to bend, straighten and rotate slightly to the left and right. Knee injuries are common and occur in all ages. It can be classified into overuse or traumatic injuries.
There 4 ligaments that are in the knee: anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL) and lateral collateral ligament (LCL). A ligament is a fibrous tissue that connects bones to other bones and determines the amount of mobility of a joint.
Ligaments can be injured through a sudden big change in direction such as a bad landing after jumping or a sudden blunt force to the knee (football players). Knee ligament injuries are more common than any other type of knee injury pathology.
It has been estimated that 2 out of 1000 people have knee ligament injuries and even more for those involved in sports. There are various types of knee injuries that can occur around the knee as a result of sporting activities and various factors affecting the area.
Overuse injuries
- Patellofemoral pain – is the most common knee pain. It presents as pain that is behind or around the patella and increased with a movement that requires bending of the knee. Risk factors include overuse, trauma, and weak or tight muscles. It is usually diagnosed by patient history and examination of the knee alone but may require imaging studies in those with a history of trauma, surgery or non-improvement despite treatment. Treatment includes rest and physical therapy. Other treatments such as analgesics and bracing have little evidence supporting their effectiveness.
- Bursitis of the knee – can also occur when the bursa becomes inflamed due to injury, excessive pressure or overuse. The inflammation of a bursa is called bursitis. Bursae are sacs that are in joints and positioned between bones and soft tissue to reduce friction. The most common symptom is a pain on the inner side of the knee which is worse when going up or down the stairs. Treatment includes physical therapy, cold packs, heat packs, analgesics, and rest.
- Patellar tendinopathy – occurs when the patella tendons degenerate. Its main features are pain that is localised right below the kneecap and increased with weight-bearing. It is diagnosed through patient history and examination of the knee. Imaging can be helpful to include or exclude other diagnoses. Treatment is rest and rehabilitation and aims to progressively increase the weight tolerance.
- Osteoarthritis – is degeneration of the cartilage in the joint resulting in the bones rubbing against each other. Risk factors include age, overweight and history of knee trauma. Symptoms include pain on activity, limited range of movement, stiffness, and swelling around the knee. It is diagnosed via examination of the knee and x-rays. Treatment includes analgesics, exercise, weight loss and physical therapy. Joint supplements such as glucosamine may also help. Knee replacement surgery is a last resort.
Acute Injuries
- Muscle strains – are pulled muscles that occur most frequently in sports. Rest, ice and compression are good first aid measures. Analgesics can also be used. Evaluation by a clinician should be done if there is the inability to move the knee, swelling or pain that lasts longer than two weeks without improvement.
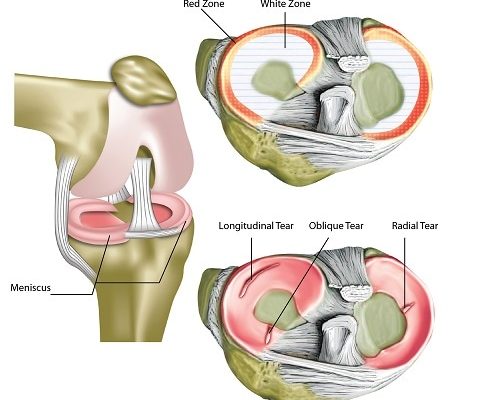
- Meniscus tear – is tear of the discs located between the two bones of the joint. The discs are cartilages that function to absorb shock. Traumatic tears are common in young athletes while degenerative tears occur in advancing age or those with arthritis. Symptoms include pain that may occur after activity accompanied by swelling. Treatment can be conservative if asymptomatic or may require surgery.
- Fractures and dislocation – of the knee can be caused by falls from significant heights and accidents. A dislocation occurs when the bones are misaligned. Symptoms include an inability to move or walk. It is diagnosed using X-rays, CT scan and MRI. Treatment may include reduction (bones are realigned), stabilisation (bones are held together to prevent any other misalignment), surgery and pain medicine. Rehabilitation can then be carried out accordingly.
Ligament Injuries
This is the most common knee injury type to affect athletes and sports professionals. Most common symptoms include swelling of the knee, pain and a sensation of the knee “giving way” during certain movements.
Injuries to the collateral ligaments usually heal with rest, bracing and rehabilitation while cruciate ligament injuries may require surgical intervention.

Anterior Cruciate Ligament (ACL) Injury
The ACL functions to prevent the tibia from sliding forward of the femur.
- Risks: Females are more likely to have ACL injuries compared to males and the number of injuries in athletes younger than 18 years has increased over the past 2 years. This may be due to increased participation of adolescents in sports and increased awareness of ACL injuries. Risk factors include genetics, hormones, previous injury, age, female gender and higher body mass index (BMI).
- Symptoms: The patient usually has symptoms of pain, swelling, reduced movement and difficulty bearing weight. A “pop” is also often heard or felt and a sensation of instability as if the knee is “giving way”.
- Diagnosis: The diagnosis is made via examination of the knee and imaging to help include and exclude other conditions
- Treatment: Treatment usually includes surgical and non-surgical options. It is found that rehabilitation with an option of delayed surgery was found to reduce the number of surgeries needed. Non-surgical options (rehabilitation) can be used for patients who are not active in sports. Indicators of surgery would be the inability to participate in their chosen sport, or an instability that affects their daily living, and involvement of other injuries in the knee joint. Patients should also be made aware that they are at increased risk of early onset osteoporosis in the injured knee regardless of treatment choice.
Posterior Cruciate Ligament (PCL) Injury
The PCL functions to prevent the tibia from sliding backwards of the femur. Injuries to the PCL alone are uncommon and are often associated with other pathologies.
- Risk Factors: It is reported that 45% are related to traffic accidents while 40% to sports injury and males are more frequently involved than females possibly due to the type of injuries and sports involved.
- Symptoms: include poorly localised pain at the back of the knee, minimal swelling and a sensation of instability. It can be diagnosed via patient history, examination of the knee and imaging.
- Treatment: The treatment of PCL injuries includes non-surgical (rehabilitation) and surgical options. Non-surgical treatment is for patients with mild symptoms or low activity needs. Surgical treatment is for highly competitive athletes or for those whom non-surgical treatment has little or no improvement.
Medial Collateral Ligament (MCL) Injury
The MCL functions to stabilise the knee (keeps it from sliding inwards) and allowing it to rotate.
- Risk Factors: Most MCL injuries occur in young people who are active in sports. It has been reported to be 0.24 per 1000 and twice as high in males compared to females.
- Symptoms: Symptoms include pain on the inner side of the knee, feeling of instability, hearing a “pop” sound, possible swelling and bruising. Patient history, examination of the knee and some imaging studies (MRI) are used to make a diagnosis of MCL injury.
- Treatment: Most MCL injuries are non-operable and can be managed conservatively by bracing and physical therapy. There are some studies that have reported no advantages of surgical intervention over non-surgical option. Bracing has been proven as an effective way to reduce MCL injury rates.
Lateral Collateral Ligament (LCL) Injury
The LCL functions to stabilise the knee (outer side of the knee). It occurs with other ligament injuries and is usually seen with a dislocated knee.
- Symptoms: Symptoms include swelling, pain on the outer side of the knee and instability. It is diagnosed using patient history, examination of the knee and imaging studies.
- Treatment: The treatment for MCL injuries are non-surgical and surgical options. Non-surgical options include bracing, the use of crutches to avoid weight-bearing and rehabilitation.
The general first aid measure for most acute knee injuries such as those above include rest, ice, compression, and elevation. Analgesics can also be used to reduce the pain in these injuries. The goal for any competitive athlete who had an injury is to allow them to return early to their sport with minimal injury and a decreased risk of recurrence.
Although the treatment plan may differ, the same goal applies to other patients, allowing them to return to their routines and reducing future recurrences of knee injuries. A tailored treatment and rehabilitation plan should also be made for each patient including steps to prevent future recurrence.
[trx_infobox style=”info” closeable=”no” bg_color=”#F9F9F9″ top=”inherit” bottom=”inherit” left=”inherit” right=”inherit”]
SOURCES
[1] Kulowski J. Flexion contracture of the knee. Journal of Bone & Joint Surgery. 1932; 14(3):618-663.
[2] Miyasaka KC, Daniel D, Stone ML. The incidence of knee ligament injuries in the general population. American Journal of Knee Surgery. 1991; 4:3-7.
[3] Ellison A, Berg G. Embryology, anatomy and function of the anterior cruciate ligament. Orthopaedic Clinic of North America. 1985; 16:3-14.
[4] Anderson AF, Snyder RB, Lipscomb Jr. AB. Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. American Journal of Sports Medicine. 2001; 29(3):272-279.
[5] Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. American Journal of Sports Medicine. 1995; 23(6):694-701.
[6] Powell JW, Barber-Foss KD. Sex-related injury patterns among selected high school sports. American Journal of Sports Medicine. 2000; 28(3):385-391.
[7] Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clinical Journal of Sports Medicine. 2006; 16(6):500–513.
[8] Arnoczky SP. Anatomy of the anterior cruciate ligament. Clinical Orthopaedics Related Research. 1983; (172): 19–25.[/trx_infobox]


![Temporomandibular_Joint-min[1]](https://www.sportnova.co.uk/wp-content/uploads/2016/07/Temporomandibular_Joint-min1-479x400.jpg)