The term “piriformis syndrome” is an abnormal condition that can be defined as a group of symptoms that are caused by the piriformis muscle, which is a muscle located in the buttocks behind the hips. The piriformis muscle primarily acts as a hip external rotator, allowing the leg and feet to rotate outwards, but is also a weak hip abductor (allowing the legs to lift sideways) and a weak hip flexor (allowing the legs and knees to be brought up towards the body). It also helps to stabilize the hips during walking and while standing.
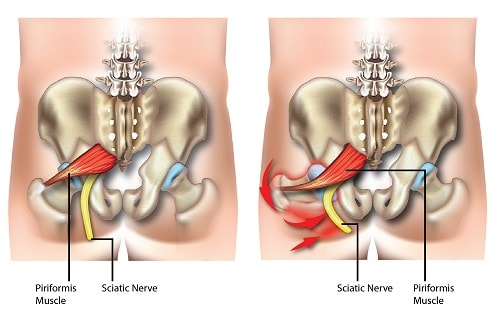
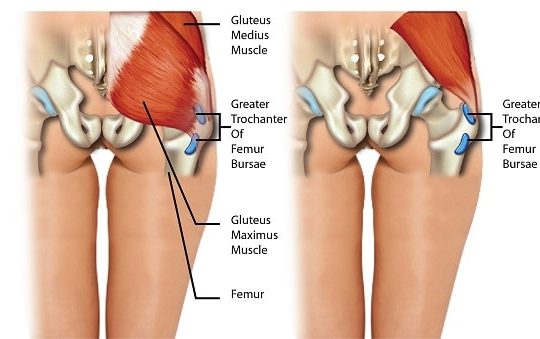
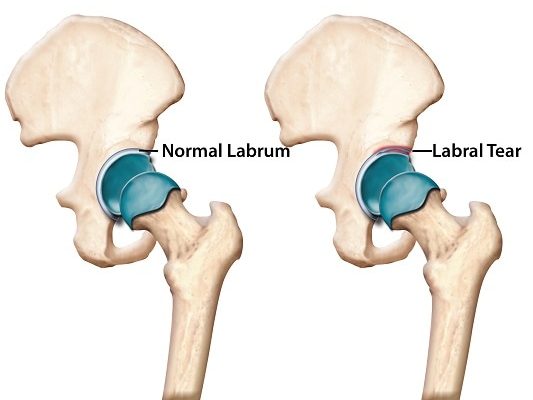
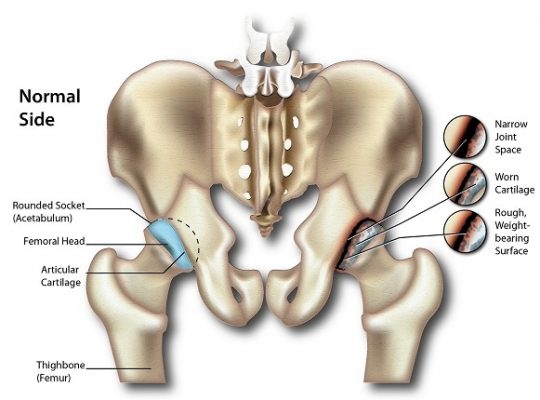
When the term piriformis syndrome is used, it also usually implies that the symptoms are caused by compression of the sciatic nerve, which is the longest nerve in the body, by the piriformis muscle. It is usually misdiagnosed, as symptoms are similar to more common pathologies such as trochanteric bursitis and lumbar radiculopathy (pinched nerve in the lower back).
Cases can be categorized as primary or secondary piriformis syndrome, based on whether the cause. For primary piriformis syndrome, the cause is anatomical, for example, the sciatic nerve piercing the piriformis muscle itself, which occurs in less than a third of the general population. For secondary piriformis syndrome, the disorder results from some other underlying factor such as micro- and macrotrauma and localized restriction of blood supply or ischemia. Less than 15% of all diagnosed piriformis syndrome cases have primary causes.
Piriformis syndrome patients are usually between 40 and 50 years old and can affect individuals at any activity level. A wide-range estimate of 5-36% has been reported for the incidence rate of piriformis syndrome in adults diagnosed with lower back pain.
SYMPTOMS
Common symptoms of piriformis syndrome are:
- Pain – it is usually experienced when immobile in a sitting, standing, or supine (lying down) position for an extended period of time (15 minutes or more). Getting up from a seated or squatting position may also induce pain. The pain however improves with walking. It may be felt from the abdomen, buttocks, pelvis, and groin, and may radiate down the back of the thigh, stopping just above the knee.
- Difficulty walking
- Foot numbness
- Headache
- Neck pain
- Weakness in the lower extremity – this is experienced on the same side of the body with the condition.
- Painful sexual intercourse for women
- Pain with bowel movement
RISK FACTORS
Common risk factors of piriformis syndrome are:
- Preceding fall or another cause of injury to the buttocks. Acute trauma may result in swelling and subsequent scar tissue formation between the sciatic nerve and the small hip extensor muscles.
- Overuse of the piriformis muscles. This can be due to unaccustomed walking, running, squatting, kneeling, cycling, etc.
- Leg length discrepancy. This may be due to structural factors, such as shortening of the bone structures, or altered biomechanical factors, which encompasses movement of the body and how forces on it during movement.
- Narrowing of the spinal canal in the lower back (Lumbar spinal stenosis)
- Muscle pain syndrome
- Piriformis muscle infection
- Cervical cancer that has invaded the piriformis muscle
DIAGNOSIS
A physical examination usually reveals tenderness in the buttocks, and tenderness to the piriformis on examination of the pelvis. Contraction of the piriformis muscle may cause a mass to be felt in the buttock, and can also cause the hip to rotate external so that if the patient lies down and is relaxed, the foot on the affected side rotates externally (this is a positive “piriformis sign”). Efforts to rotate the foot to midline position would cause pain (Freidberg test). Other tests that are usually conducted, and positive (that is, pain is elicited) if the patient does have piriformis syndrome are:
- FAIR (flexion, adduction and internal rotation) test – for this test, the patient is lying on the unaffected side, with hips flexed at 60o and knees flexed at 60 to 90o. The examiner then internally rotates the affected hip by applying downward pressure to the knee. It can also be carried out with the patient lying down on their back or in a seated position.
- Straight leg raise (Lasègue) test – this is done by having the examiner lift the straightened leg while the patient is lying down.
- Beatty test – for this test, the patient is lying down on the unaffected side and instructed to lift and hold the knee of the affected side about 4 inches above the examination table.
- Electromyography (EMG) – may also be used when making a diagnosis for piriformis syndrome. Patients with piriformis syndrome would have normal EMG results for muscles situated near the piriformis muscles but abnormal for muscles situated further away from it. Imaging techniques are limited in making a diagnosis for piriformis syndrome, but would be helpful in eliminating other possible pathologies.
TREATMENT
Treatment should commence as soon as possible, as early conservative treatment effectively reduces symptoms in most patients. One study reported that 79% of patients had a reduction in symptoms after a treatment regime of non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, ice, and rest. Acetaminophen is also commonly prescribed.
Stretching and strengthening of the piriformis muscle, the abductor muscles, and adductor muscles is also recommended.
Surgery is a last resort option, for patients that have not responded well to conservative treatment.
SOURCES
[1] NIH. (2007) NINDS Piriformis Syndrome Information Page.
[2] Boyajian-O’Neill, L. A., McClain, R. L., Coleman, M. K., and Thomas, P. P. (2008) Diagnosis and management of piriformis syndrome: an osteopathic approach, J Am Osteopath Assoc 108, 657-664.
[3] Siddiq, M. A., Khasru, M. R., and Rasker, J. J. (2014) Piriformis syndrome in fibromyalgia: clinical diagnosis and successful treatment, Case Rep Rheumatol 2014, 893836.