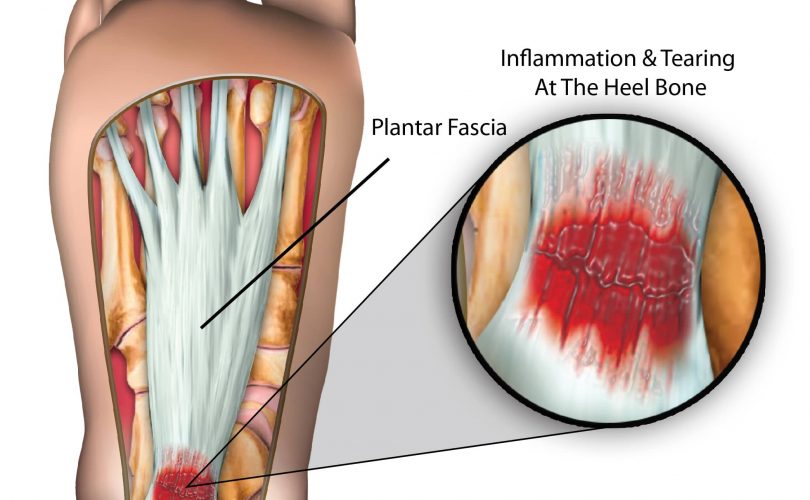
What is plantar fasciitis?
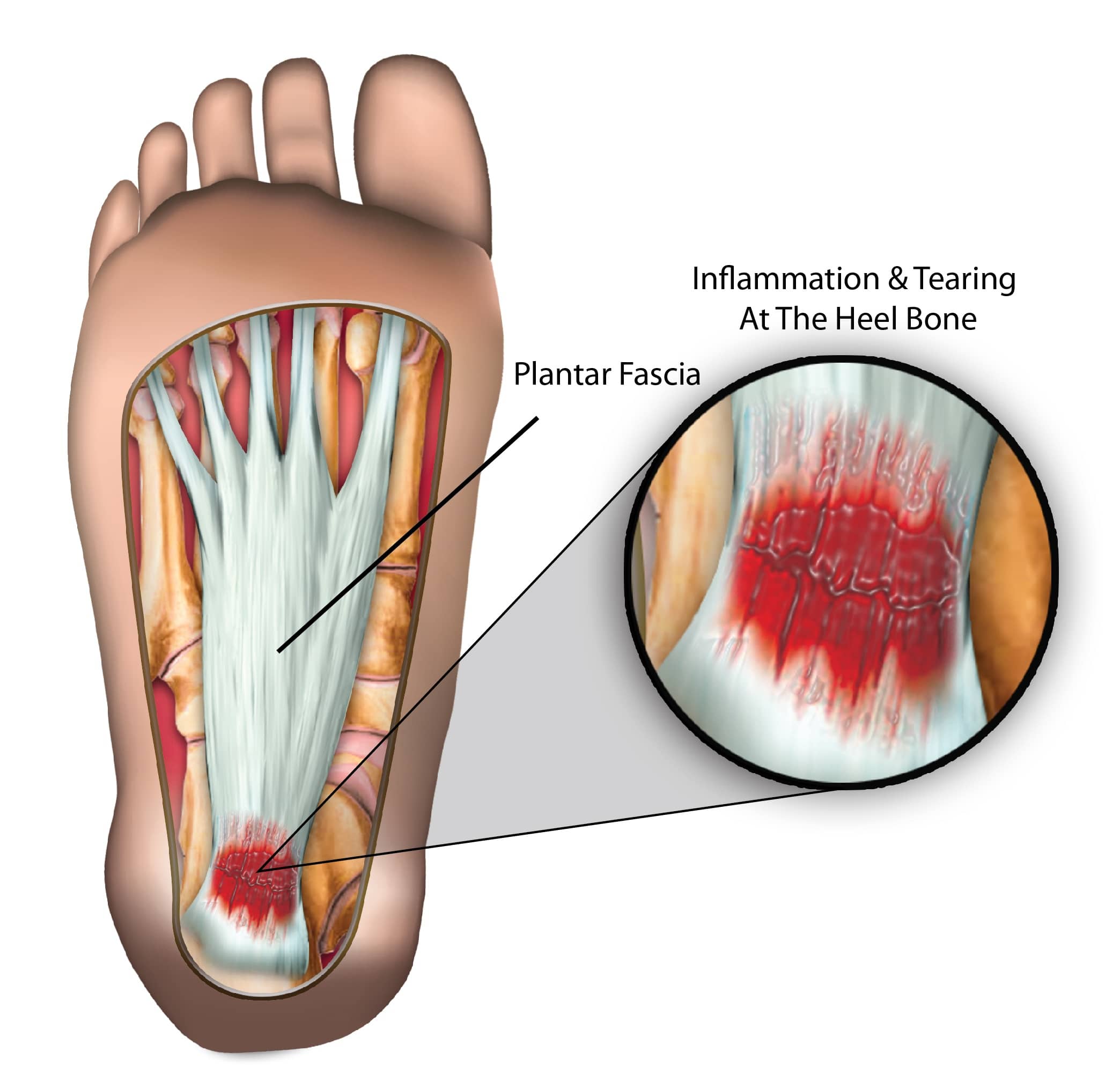
Plantar fasciitis is a common condition that occurs when the the plantar fascia ligament which stretches the heel to the toes becomes inflamed, causing pain. This is understood to be the leading cause of heel pain in the UK.
As the majority of people walk across their lifetime, the foot region experiences general wear and tear and the plantar fascia acts as a cushion supporting the arch of the foot. When the foot experiences too much pressure, the plantar fascia can become damaged and inflamed causing pain and stiffness.
What are the symptoms of plantar fasciitis?
This condition is usually characterised by a mild, gradual pain at the bottom of the foot usually near the heel (sometimes misdiagnosed as a heel spur) and might then radiate through to the centre of the foot sole.
The other symptoms of plantar fasciitis include:
- Slight or severe pain when pressure is applied to the sole of the feet
- “First step pain” which usually occurs in the morning when waking
- Pain when standing after long periods of idleness
The pain is usually most prominent during the morning as the plantar fascia has been relaxed during the night, but is then suddenly utilised again when getting up. As the plantar fascia stretches out and warms up the pain usually lessens.
What are the causes of plantar fasciitis?
Plantar fasciitis usually occurs as a result of repetitive over-extension of the plantar fascia. It can therefore be referred to as a overuse injury. Although traditionally it is thought that the condition causes inflammation, it has been found that due to the absences of inflammatory cells present in the fascia, the condition occurs most likely due to degeneration or tearing of the plantar fascia.
This condition is also most likely to occur if a person:
- overstretches the sole of the foot
- wears shoes with the wrong fitting
- exercises on hard surfaces
- lands heavily repetitively with and exposed sole
What are the risk factors associated with plantar fasciitis?
Although the condition is mostly common in active sportspeople or those who participate in activities such as running or dancing, it can also occur in the average human being.
There are certain factors that can increase the likelihood of this condition such as:
- Being very overweight – this means increased load on the foot which is likely to lead to pain
- Flat foot or over pronation – the tissue of the plantar fascia is strained as it is stretched more than due to the flat foot
- Tight ankle tendons – such imbalances can pre-dispose individuals to also suffer the same with the plantar fascia
- High arched feet – can cause a strain at the fascia attachment due to the rigidity and lack of support
- High intensity sport – involvement in sports that requirement repetitive foot movement at high impact
- Gender – although men can develop plantar fasciitis, it is said to be more prominent in women.
How is plantar fasciitis diagnosed?
The diagnosis of this condition is usually carried out by a doctor or an orthopaedic specialist. An initial assessment will help in discovering the individual’s general health and any previous and current injuries that may have been sustained to the area.
Tests are carried out to confirm the injury and its stage, these tests include:
- Range of motion – carried out in order for doctor to know how limited the motion of the foot from the ankle is and at which point the pain begins or stops.
- Posture – the doctor is likely to study how the individual stands and walks, looking in particular to the arch of the foot. Flat feet (overpronation), oversupination or a high arch are said to contribute to plantar fasciitis
- Pain and inflammation – a closer inspection of the sole of the feet is carried out, and is felt (palpated) to confirm where the pain epicentre is and possibly any soreness of the area.
What are the treatments for plantar fasciitis?
Treatment for this condition normally involves the combination of various pain relief methods such as:
- Pain killers – over the counter treatments and NSAIDs (anti-inflammatory medication) are useful in decreasing pain and inflammation.
- Stretching – light stretching of the foot and heel a few times a day can be done to ensure the tissue becomes flexible and not stiff after injury
- Orthopaedic footwear – gaits and heel pads have been known to help reduce the chance of plantar fasciitis reoccurring
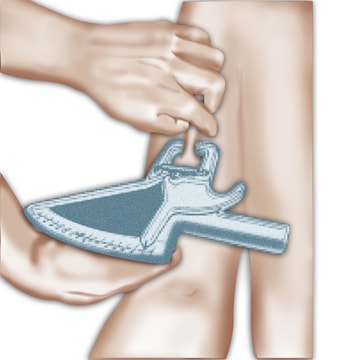
- Splint – a night splint is often used to prevent the plantar fascia for shortening during the night as the foot is kept in place at a certain angle
How to treat plantar fasciitis yourself?
If there is a sudden onset of the condition, then certain steps are adviced to reduce pain and prevent further degradation or inflammation. It is recommended:
- R.I.C.E (Rest, ice, compress, elevate) principle – the foot should be elevated and wrapped in ice for between 15-20 mins every few hours. Cold packs and hot packs can also provide a similar benefit.
- Change footwear – find wide and comfortable shoes with a soft sole
- Take paracetamol
- Do not stand for long periods of time
- Apply warm lavender oil to the sole of the foot due to its anti-inflammatory properties
- Do not take ibuprofen for the first few days
- Do not walk barefoot or in slippers
Alternative treatments for plantar fasciitis
More direct medical treatments for plantar fasciitis include:
- Ultrasound therapy – gentle sound waves are emitted on the area to reduce inflammation
- Shockwave therapy – normally used if there is consistent pain for over 4-6months, wherein a high intensity wave is released to aid healing of the area.
- Steroidal injections – an anti-inflammatory injection is applied directly to the site of the pain which may temporarily provide relief around the heel and sole. This method though should be limited in its use.
These are usually not required and are used as a last resort if the foot is not responsive to other treatment methods.
How to prevent plantar fasciitis from reoccuring?
There are certain steps that can be taken to reduce the risk of plantar fasciitis, these include:
- Wearing the correct footwear – ensuring that footwear is not too old with a worn out sole is important. Shoes with adequate cushioning are better at protecting the plantar fascia
- Protective covering – taping the foot adequately can help the recovery process and support it after an injury
- Stretching – flexing and rotating the muscles in the lower leg can help in conditioning the plantar fascia properly
- Gradual training – when returning from injury, a measured training approach is essential in order to prevent a reoccurrence of the injury
- Apply ice – icing the foot after training can help to reduce any sudden inflammation and lower overall pain
- Losing weight – less strain on the foot means less likelihood of there being inflammation in the plantar fascia.
Exercises to help prevent plantar fasciitis
Certain types of exercise can help to prevent the occurence or reoccurence of plantar fasciitis, these include:
- Calve stretches – this exercise helps to losen the soleus muscle in the lower calf improving flexibility and strength around the plantar fascia
- Foot roll – whilst sitting down, roll the affected foot on a foam roller or a cold can/bottle. This not only helps to reduce inflammation but also relieve the painful area
- Toe stretches – whilst sitting down, stretch out the affected foot slightly, grab your big toe and pull towards the body, hold this for 10-15 seconds, do this 3-4 times
FAQS
Q. What is the recovery time for plantar fasciitis?
A. As long as the plantar fascia tissue is not degenerating, average recovery time can be between 3 weeks to 5 months. This is dependent on the level of the injury and the treatments being carried out
Q. Is plantar fasciitis the same as plantar fibroma?
A. No, plantar fibroma is much less common than plantar fasciitis and occurs when a benign fibrous tissue grows in the arch of the foot. Although the symptoms are slightly similar, there is no nown cause for plantar fibroma.
Q. What is ‘Policeman’s Foot’?
A. Policeman’s foot is another term used to describe plantar fasciitis
Q. Do home remedies work for plantar fasciitis?
A. There are some natural remedies with anti-inflammatory properties which help in reducing paid in the affected area such as lavender oil and apple cider vinegar. There are however other unverified remedies such as mustard and aloe-vera which are said to be helpful.