What are shin splints?
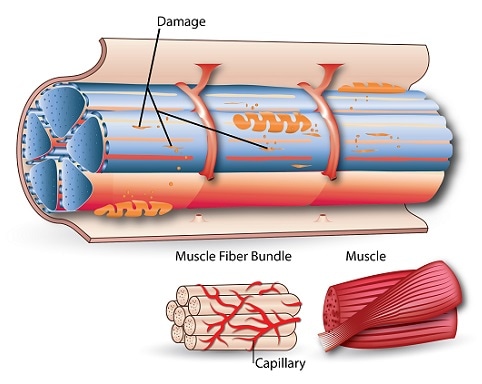
Shin splints or medial tibial stress syndrome (MTSS), is an overuse injury caused by repetitive stress on the muscles and tendons around the shinbone (tibia). It is often characterised by pain felt in the lower two-thirds of the shinbone and is brought on by running or other activities that apply constant load on the tibia. Where there is inflammation alongside pain before or after exercise is referred to as periostitis.

Shin splints share common characteristics to stress fractures of the shinbone as it is a stress-induced reaction. While they do share similarities, shin splints often occur in areas on the shinbone where stress fractures are not found. Additionally, many cases do not become stress fractures and as such should be treated as separate conditions.
It is also commonly seen in other sports such as basketball, football, and dancing.
Risk factors of shin splints
Shin splints can often be categorised via extrinsic, intrinsic, historical and gender related factors. Extrinsic factors include:
- High frequency and intensity of training
- The training surface e.g. running on hard, uneven surfaces such as a pavement or road
Intrinsic affect how the load is applied on the lower extremities of the body:
- Increased Body Mass Index (BMI), results in increased load bearing.
- Hyperpronation – pronation is the natural reaction when walking or running, where the foot, flat on the ground, rolls inwards for stabilization. Hyperpronation however, can put pressure on the medial or inner sections of the shinbone causing inflammation
- Having flat feet
- Stress fractures
Historical risk factors of shin splints include:
- Prior use of orthotics or shoe inserts
- History of shin splints – those with previous cases of MTSS (shin splints) have a significantly higher risk of recurrence cases.
- Fewer years spent actively participating in running – this is likely to be due to lower neuromuscular and bone adaptation to the sport, as the body is constantly conditioning itself based on present mechanical load demands.
Gender factors:
- Overall, females are more at risk of developing shin splints than males – this is due to biological dispositions affecting leg length and differing strength of the tibia
Symptoms of shin splints
The main symptoms of shin splints are:
- Pain brought on by exercise, but not present when at rest.
- Inflammation of the periosteum
If the pain is intense, it is recommended to stop activity and rest the affect area to prevent any further damage.
How do you diagnose shin splints?
The diagnosis of shin splints can usually be done by the individual after experiencing the symptoms mentioned. In cases of uncertainty, the individual can seek clinical advise. Observation and palpation of the area will take place to feel for localised tenderness between the middle and lower third of the shinbone. The physician can then determine if the injury can be diagnosed as shin splints.
In cases where there is not a conclusive result, an MRI scan may be carried out as it could aid in detecting other issues such as periostitis.
How do you treat shin splints?
Treatment of shin splints varies according to the cause and the injury, but is typically non-surgical, with rest, ice and supportive footwear most frequently prescribed. Stretching regularly and strengthening the calf and glutes are also know to help in recovery and preventing of the condition.
Recovery from MTSS tends to take several weeks to several months. In rare cases, individuals suffering with chronic shin splints may have to undergo surgery.
SOURCES
[1] Ringdahl, E., and Pandit, S. (2011) Treatment of knee osteoarthritis, Am Fam Physician 83, 1287-1292.
[2] Arthritis Research UK. R. (2013) Osteoarthritis in general practice.
[3] Stiebel, M., Miller, L. E., and Block, J. E. (2014) Post-traumatic knee osteoarthritis in the young patient: therapeutic dilemmas and emerging technologies, Open Access J Sports Med 5, 73-79.
[4] Cattano, N., Barbe, M., Massicotte, V., Sitler, M., Balasubramanian, E., Tierney, R., and Driban, J. (2013) Joint trauma initiates knee osteoarthritis through biochemical and biomechanical processes and interactions, OA Musculoskeletal Medicine 1, 3.
[5] Arden, N. K., Arden, E., and Hunter, D. (2008) Osteoarthritis, Oxford University Press.
[6] Nature. Nature Reviews: Rheumatology.