Spondylolysis and spondylolisthesis are two key causes of lower back pain, especially in many young sports professionals.
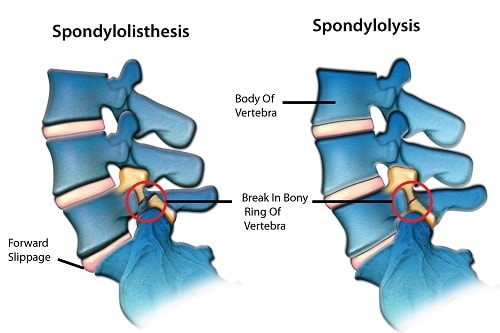
Spondylolysis is caused when there is a crack or stress fracture, in the region of the vertebra called the “pars interarticularis” that forms the joint in the spine. It typically occurs in young athletes who participate in sports such as basketball, football, rugby and gymnastics, which put repetitive strain on the lower back. If left untreated, the vertebra can slip out of place and then develop into a condition called spondylolisthesis.
Spondylolisthesis occurs when there is a forward displacement of a vertebra over the vertebra below it, disrupting the natural curvature of the spine. It is an advanced cause of lower back pain and has six main types.
- Dysplastic or congenital spondylolisthesis – this is when spondylolisthesis is due to a birth defect, such as spina bifida and scoliosis.
- Isthmic spondylolisthesis – this occurs from the progression of other spinal injuries, mainly spondylolysis.
- Degenerative spondylolisthesis – this is the most common type of spondylolisthesis and is due to chronic degeneration in the vetebra. It is usually seen in individuals over 50 and is usually caused by arthritis.
- Traumatic spondylolisthesis – this is when spinal destabilization is caused by acute trauma such as a sharp blow to the back or fall.
- Pathologic spondylolisthesis – this is when spondylolisthesis occurs as a result of a disease that affects the bones.
- Post-operative spondylolisthesis – this occurs from complications due to surgery, with an incident rate of about 3-5% of all treated spondylolisthesis.
What are the symptoms?
In many cases, individuals with spondylolysis and spondylolisthesis rarely have any obvious symptoms until they engage in sporting activity which aggravates the lower back. When there are symptoms, these are usually:
- Lower back pain
- Localised tenderness
- Weakness in the legs
- Pain, tingling or numbness in the thighs and buttocks (similar to sciatica)
- Stiffness
Advanced cases of spondylolisthesis may result in difficulty walking and tightness in the hamstring muscles
What are the causes and risk factors?
Common risk factors of spondylolysis and spondylolisthesis include:
- Congenitally dysplastic joints – children born with underdeveloped facet joints in the spine may experience the forward slippage of a vertebra. This can also cause the compression of a nerve.
- Hyperextension of the lumbar spine – this is usually the cause for the progression of spondylolysis to spondylolisthesis. Hyperextension can be due to weak pars interarticularis, abnormal bone healing or trauma.
- Degenerative bone disease – degenerative bone diseases, such as arthritis, that result in instability in the vertebra can lead to slippage.
- Trauma – trauma can lead to fractures and dislocation of various components of the spine.
- Gender – studies show that women are four times more likely to develop spondylolysis than men.
- Genetics – there is an increased chance of having spondylolysis or spondylolisthesis, if other family members have also suffered from it.
How is it diagnosed?
The severity of spondylolysis and spondylolisthesis can be categorised in six stages, depending on the extent of displacement of the vertebra:
Stage I – initial stress fracture
Stage II – complete stress fracture
Stage III – displacement of 0-25%
Stage IV – displacement between 26-50%
Stage V – displacement between 51%-75%
Stage VI – displacement between 76%-100%
Diagnosis is usually made from a physical examination by a doctor, where the affected area is assessed for motion, tenderness or weakness. The doctor may also assess the posture or walking movement of the individual, as these are key symptoms in the diagnosis of spondylolysis and spondylolisthesis.
The doctor at this point may request an X-ray examination of the spine to see if a vertebra is out of place or is at an earlier stage of a stress fracture. X-ray should be done with the patient standing instead of lying down because the degree of slippage increases to 26% when standing versus lying down.
What treatments are available?
Appropriate treatment is dependent on the degree of dislocation as well as the age of the patient. In most cases and especially for young individuals where the skeleton has not fully matured spondylolysis (grade I or II) can be treated conservatively, this includes:
- changes to lifestyle e.g. break from sports and activities that put strain on the lower back
- physical therapy that help in strengthening the back and leg muscles
- drug therapy e.g the use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.
- bracing the affected area to prevent further damage, allowing the vertebra to heal.
In individuals with grade V or VI spondylolisthesis, wherein, the condition is progressively worsening, then surgical intervention may be required. The main procedure carried out in this case is called ‘spinal fusion’. This occurs when the doctor welds the displaced vertebra back in place using bone grafts and sometimes metal screws, this will help the healing process and further stabilisation of the back.
SOURCES
[1] Jacob, E. (2013) Medifocus Guidebook on Spondylolisthesis, Medifocus.com, Inc.
[2] MedlinePlus. (2014) Spondylolisthesis.
[3] Garet, M., Reiman, M. P., Mathers, J., and Sylvain, J. (2013) Nonoperative treatment in lumbar spondylolysis and spondylolisthesis: a systematic review, Sports Health 5, 225-232.
[4] Omidi-Kashani, F., Ebrahimzadeh, M. H., and Salari, S. (2014) Lumbar spondylolysis and spondylolytic spondylolisthesis: who should be have surgery? An algorithmic approach, Asian Spine J 8, 856-863.